Plantar Fasciitis (Heel Pain)
Home / Diseases Conditions / Plantar Fasciitis (Heel Pain)
What is Plantar Fasciitis?
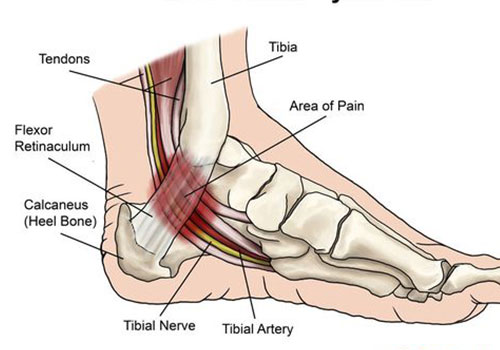
Plantar fasciitis is a common cause of heel pain, involving inflammation of the thick band of tissue (plantar fascia) that runs across the bottom of your foot, connecting your heel bone to your toes. This condition often results from repetitive strain injuries to the ligament of the sole and is especially prevalent among runners, people who are overweight, and those who wear shoes with inadequate support.
Plantar fasciitis typically manifests as a stabbing pain, especially noticeable with your first steps in the morning. As you get up and move more, the pain usually decreases but may return after long periods of standing or after getting up from sitting. This pain can significantly impact daily activities, making it challenging to walk or stand for extended periods.
Common Causes of Plantar Fasciitis
- Overuse: Activities that put excessive stress on your heel and its attached tissues, such as long-distance running, ballet dancing, and aerobic dance, can lead to repetitive microtrauma to the plantar fascia, resulting in inflammation.
- Foot Mechanics: Conditions like flat feet, high arches, or abnormal walking patterns can affect weight distribution, increasing stress on the plantar fascia and leading to inflammation.
- Obesity: Excess weight adds extra stress to your plantar fascia, increasing the mechanical load and contributing to chronic inflammation and pain.
- Occupational Hazards: Jobs requiring prolonged standing or walking on hard surfaces can damage the plantar fascia, exacerbating the condition by continually stressing the area.
Common Symptoms of Plantar Fasciitis
Symptoms of plantar fasciitis include:
- Heel Pain: A stabbing pain at the bottom of the foot near the heel, particularly after long periods of rest. The pain is usually most intense with the first steps of the day or after prolonged inactivity.
- Stiffness: Stiffness and discomfort in the heel, most severe with the first steps of the day or after sitting for long periods. This stiffness can lessen with activity but may return after standing or sitting for extended periods.
- Tenderness: Tenderness at the bottom of the foot, usually closer to the heel. This tenderness can be aggravated by pressing on the area or wearing certain types of shoes.
Risk Factors for Plantar Fasciitis
Several factors can increase your risk of developing plantar fasciitis, including:
- Age: Most common between the ages of 40 and 60. The natural aging process can decrease the elasticity and strength of the plantar fascia, making it more prone to injury.
- Foot Mechanics: Flat feet, high arches, or abnormal walking patterns can contribute to plantar fasciitis by altering weight distribution and increasing strain on the plantar fascia.
- Obesity: Excess weight adds extra pressure on the plantar fascia, increasing the risk of inflammation and pain.
- Certain Types of Exercise: High-impact activities, such as long-distance running, ballet dancing, and aerobic dance, can increase the risk of plantar fasciitis by causing repetitive microtrauma.
- Occupation: Jobs requiring extensive walking or standing on hard surfaces can exacerbate the condition by continually stressing the plantar fascia.
How to Diagnose Plantar Fasciitis
- Physical Exam: Check for areas of tenderness in the foot. The location of pain can help determine its cause.
- Imaging Tests: X-rays or MRIs may be used to rule out other causes of heel pain, such as fractures, and to identify heel spurs associated with plantar fasciitis.
- Medical History: Reviewing your medical history helps identify risk factors and guides the treatment plan.
Plantar Fasciitis Heel Pain Treatment
At Sports Massage Clinic, we offer comprehensive plantar fasciitis heel pain treatment in Singapore, including:
- Physical therapy: Specialized exercises to stretch the plantar fascia and Achilles tendon, helping to relieve pain and improve flexibility.
- Supportive devices: Orthotics to help distribute pressure more evenly across your feet. Custom orthotics can provide support and reduce stress on the plantar fascia.
- Medications: NSAIDs (nonsteroidal anti-inflammatory drugs) to reduce pain and inflammation in the short term.
- Surgery: In severe cases, surgical intervention may be necessary when conservative treatments fail to provide relief.
Rehabilitation and Prevention after Treatment
After treatment, it’s important to:
- Rest and ice: Allow your feet to heal by resting and applying ice to reduce inflammation. Rest prevents further injury, while ice alleviates pain and swelling.
- Proper footwear: Wear shoes with good arch support and cushioning to distribute weight evenly and reduce strain on the plantar fascia.
- Gradual return to activity: Slowly increase your activity levels to avoid re-injury. Gradual progression helps your body adapt without overloading the plantar fascia.
Stretching Exercises for Plantar Fasciitis
Incorporate these stretches into your daily routine:
- Towel stretch: Sit on the floor with your legs extended. Loop a towel around the ball of your foot and pull gently. Hold for 15-30 seconds and repeat several times.
- Calf stretch: Stand facing a wall with your affected foot behind your other foot. Lean forward into the wall to stretch your calf. Hold for 15-30 seconds and repeat several times.
- Plantar fascia stretch: Sit on a chair and cross one leg over the other. Pull your toes back towards your shin to stretch the plantar fascia. Hold for 15-30 seconds and repeat several times.
Frequently Asked Questions

